Video Summary of Testosterone Replacement Therapy and Cardiovascular Risk
- Published in Testosterone Replacement Therapy
- Written by Monica

One of the most controversial and debated issue related to testosterone replacement therapy is its effects on cardiovascular risk and related clinical outcomes.
In the February 2015 issue of Mayo Clinic Proceedings a comprehensive medical review paper, written by Dr. Abraham Morgentaler and his coauthors of the Androgen Study Group – www.AndrogenStudyGroup.org - was published.[1]
The aim of the review was to analyze all available studies on testosterone replacement therapy and cardiovascular effects, and to clarify the grossly misleading conclusions from two recent studies that caused a tremendous media scare.
In this 8 minute video, Dr. Morgentaler presents the key results from this comprehensive analysis…
Article Tags
Is Testosterone Replacement Therapy a Lifelong Treatment?
- Published in Testosterone Replacement Therapy
- Written by Monica

A common question among hypogonadal men is how long they should stay on testosterone therapy.
The answer is - it depends on what is causing a man’s testosterone deficiency..
Article Tags
Red Meat and Health - have we been blaming the wrong thing?
- Published in Diet, Nutrition & Supplements
- Written by Monica
Frequent consumption of red meant and processed meats has been shown in population studies to be associated with cardiovascular disease, cancer and type 2 diabetes [1-3]. It has also been suggested that eating meat increases all-cause mortality [4]. Hence, a high meat intake (regardless of its fat quantity and quality) is generally perceived to be unhealthy and something that should be avoided.
Article Tags
The Arginine Paradox - do L-arginine based NO boosters really work?
- Published in Diet, Nutrition & Supplements
- Written by Monica

Some of the most popular supplements today are the so called pre-workout nitric oxide (NO) boosters [1, 2]. These contain a panoply of ingredients, but one the main ones is arginine. The rationale goes that L-arginine is a nitric oxide (NO) precursor and NO is a potent vasodilator [3, 4]. Theoretically this would increase blood flow and nutrient/oxygen delivery to exercising muscles and thereby boost performance, as well as recovery.
While it is true that L-arginine supplementation may be beneficial for various clinical populations (see below), studies in healthy adults have not unequivocally supported the marketing hype surrounding arginine supplementation and nitric oxide boosters [1, 5, 6]. Why? Let's take a look under the hood...
Article Tags
Health Consequences of Subclinical Testosterone Deficiency - riskier than previously thought
- Published in Testosterone - Men
- Written by Monica

In discussions about diagnosis and health consequences of hypogonadism, aka testosterone deficiency, the prime focus is given to testosterone levels and signs/symptoms.[1-3] However, emerging research has identified a less clinically evident gonadal dysfunction called “subclinical” hypogonadism (or “compensated” hypogonadism).[4, 5]
Subclinical hypogonadism is characterized by normal testosterone levels in the presence of elevated LH level. As testosterone levels are not markedly reduced in subclinical hypogonadism, intuitively one may think it does not confer negative health consequences.
However, a recent study by Corona et al., which specifically was conducted to investigate the potential health ramifications of subclinical hypogonadism, shows that it should not be neglected. Surprisingly, subclinical hypogonadism is associated with an almost 10-fold increased risk of cardiovascular mortality, which is comparable to that for overt hypogonadism! [6]
Article Tags
Testosterone Therapy and Cardiovascular Risk - Advances and Controversies
- Published in Testosterone Replacement Therapy
- Written by Monica
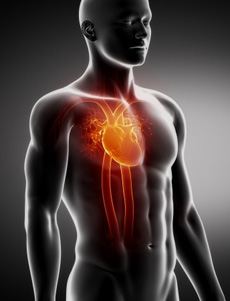
One of the most debated issues related to testosterone therapy is its effects on cardiovascular risk and clinical events, like for example heart attack.
January 27th, 2015 a comprehensive medical review paper was published, addressing the controversial topic of testosterone therapy and cardiovascular risk.[65] It was written by the Androgen Study Group academicians and published in Mayo Clinic Proceedings.
Here I summarizes key conclusions from this milestone medical review.
Article Tags
Dietary Guidelines on Fat Intake - has there ever been any evidence to support the low-fat recommendation?
- Published in Diet, Nutrition & Supplements
- Written by Monica
In an effort to slash heart disease, the Dietary Guidelines for Americans [1] have since 1977 been urging people to:
1. Reduce total fat consumption to 30% of total caloric intake.
2. Reduce saturated fat consumption to 10% of total energy intake.
Government issued dietary guidelines are highly authoritative and regarded by a majority as being backed by solid research. However, as it turns out, this is not the case…
Dietary recommendations regarding intake of total and saturated fat are highly controversial, and the debate is heating up. A recent systematic review and meta-analysis of six studies that were available 1977, when the first version of the Dietary Guidelines for Americans was published, shows: [2]
Article Tags
Testosterone, Mortality and Longevity
- Published in Testosterone Replacement Therapy
- Written by Monica

Population studies show that men with low or low-normal testosterone levels are at an increased risk of mortality compared to those with higher levels, and that cardiovascular disease accounts for the greater proportion of deaths in men with low testosterone.[1]
Here I summarize a medical review paper which addressed the following two questions: [1]
1. Is testosterone deficiency directly involved in the pathogenesis of these conditions or is it merely a biomarker of ill health and the severity of underlying disease processes?
2. Does testosterone replacement therapy retard disease progression and ultimately enhance the clinical prognosis and survival?
Article Tags
Testing for testosterone deficiency - things to know about the blood draw
- Published in Testosterone Replacement Therapy
- Written by Monica
The first step (aside from identifying symptoms) in diagnosing testosterone deficiency, aka low-T, is to do a blood test.
Here I cover some important practical things to know about a blood draw for testosterone analysis...

Article Tags
Fish Oil for Muscle Growth and Prevention of Muscle Loss with Aging
- Published in Diet, Nutrition & Supplements
- Written by Monica

A key hallmark of aging is a progressive loss of muscle mass, which occurs independently of health status.[1] Exercise and nutrition are the two main anabolic stimuli for muscle growth and its maintenance throughout the life course.[2-11]
It is clear that maintaining high physical activity and exercise levels throughout ones lifespan reduces aging related loss of muscle mass and function, compared with living a sedentary life.[12-19]
However, even active older adults and master elite athletes still experience some loss of muscle and physical performance with advancing age.[8, 13, 20]
When it comes to nutrition, high protein intake [2, 3, 10, 21] and creatine supplementation [4-8, 22] are two of the best documented interventions, which together with resistance exercise training, result in greater increases muscle mass and strength in both young [21-23] and older people [2-8, 10], and prevent its loss with aging. Here I will present the relatively unknown effevts of fish oil (most well-known for its cardiovascular health promoting effects) on muscle growth (anabolism) and its possible contribution to prevention of aging related loss of muscle mass and function...
Article Tags
More...
- Cardiovascular Risks and Elevations of Blood DHT Levels Vary by Testosterone Preparation
- Testosterone and Fat Loss - the Evidence
- Testosterone Thresholds and Muscle Mass Gains Needed to Enhance Muscle Strength and Function
- Testosterone Therapy Prevents Gain in Intra-Abdominal Fat and Counteracts Loss of Muscle in Non-Obese Aging Men



