Testosterone - Men
6 Best Foods to Help Increase Low Testosterone
- Published in Testosterone Replacement Therapy
- Written by Christine Le

Having adequate levels of testosterone is a vital factor in determining your quality of life. For beginners, testosterone is a male sex hormone found in men and women found to be important for energy, fertility, healthy sexual functions, and building muscle. Testosterone is one of the main causes of physical changes for boys during puberty, like promoting deeper voice and hair growth. Generally, a person’s testosterone level will steadily decline as you age, depending on medical conditions, lifestyle choices, and other factors. A decreasing T level can result in a lot of changes in your body, including a lower sex drive.
Article Tags
5 Signs Your Testosterone is Too Low
- Published in Testosterone Replacement Therapy
- Written by Christine

Like all hormones, testosterone plays an important role in regulating a host of different processes in the body. There is no question maintaining optimal levels of testosterone is ideal to a healthy lifestyle. Testosterone is an essential hormone responsible for male development, masculine characteristics, building muscle, fueling sex drive, and receptors exists throughout the body. This hormone is primarily produced in the male testicles and womens’ adrenal glands. As we age, testosterone production begins to slow down. If you have low levels of testosterone, the consequences can greatly affect your health.
Article Tags
5 Ways to Naturally Boost Your Testosterone
- Published in Testosterone Replacement Therapy
- Written by Christine
When you see the term “testosterone,” we typically associate it with masculinity and men. However, women generate testosterone too. So, what exactly is testosterone? Testosterone is a steroid hormone that plays a significant role in the male sperm production and produced in women’s ovaries in much smaller amounts. Rising levels of testosterone stimulates physical and chemical changes for boys and men such as increased muscle, pubic hair growth, deeper lengthened vocal chords, and increased sexual desire.
Testosterone production significantly spikes during puberty and starts to drop after age 30. Having optimal levels of the steroid hormone is essential from puberty throughout adulthood for general health, aids in preventing certain chronic diseases, and increases energy levels. As our levels of testosterone naturally decrease over time, rest assured there are ways to naturally boost it back up.
Article Tags
Hematocrit (blood thickness) elevation following testosterone therapy – does it increase risk of blood clots?
- Published in Testosterone Replacement Therapy
- Written by Monica

In discussions about side effects of testosterone treatment, prostate cancer and heart disease get most attention. However, as we have described in several study reports published here in the “Research News” section, the widespread fear of prostate cancer and heart disease is unfounded and not supported by medical research.
The expected potential side effect of testosterone treatment - which in fact is a therapeutic effect in men with anemia [1-3] - is an increased level of red blood cells, known as erythrocytosis or polycythemia.[4-7] In the context of testosterone treatment, erythrocytosis and polycythemia are used interchangeably to refer to an abnormal increase of red blood cells or hematocrit, which may increase blood viscosity (“blood thickness”).[8, 9]
However, it should be pointed out that technically, erythrocytosis is just red blood cell elevation, while polycythemia involves elevation of red blood cells, white blood cells, and platelets. Using these terms as synonyms can cause confusion. In polycythemia, it is likely the increase in platelets that is the major culprit of blood clots.
Elevated hematocrit is the most common side-effect of testosterone treatment.[4-7] The clinical significance of a high hematocrit level is unclear, but it may theoretically be associated with an increased risk of thrombosis (blood clots).[4]
Here I summarize the results of an analysis of the effect of different testosterone preparations on hematocrit elevations, published in the journal Sexual Medicine Reviews.[10]
Article Tags
Is there a protective role of testosterone against high-grade prostate cancer?
- Published in Testosterone Replacement Therapy
- Written by Monica
Historically, testosterone has almost been a synonym for prostate cancer, and therefore many men have been - and still are - denied testosterone therapy, despite having testosterone deficiency.[1]
A rapidly growing number of studies have challenged the long-standing belief about a putative detrimental association between testosterone and prostate cancer development and/or progression.[2-5] Here I summarize the results of a study published in The Aging Male, which investigated the incidence and severity of prostate cancer in testosterone treated versus non-testosterone treated patients who underwent prostate biopsy.[1]
Article Tags
Effects of testosterone treatment on body fat, lean mass, symptoms and leptin resistance in obese men on a calorie-restricted diet
- Published in Testosterone Replacement Therapy
- Written by Monica
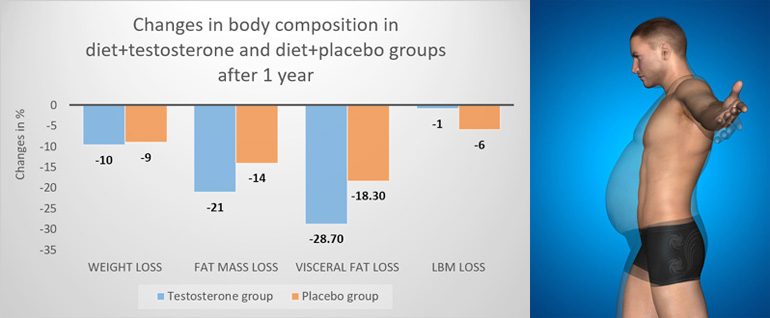
It is well-documented that the relation between testosterone deficiency and body fat is bi-directional; low testosterone levels contribute to the development of excessive body fat accumulation, and an excessive amount of body fat contributes to a reduction in testosterone levels.[1-3]
Here I present a series of three reports from a study that specifically investigated if testosterone therapy has beneficial effects on body composition, symptomatic response, adipokines (hormones secreted by fat cells, such as leptin and adiponectin) and gut hormones, over and above caloric restriction alone.[4-6]
Key Points
- Compared to diet alone, combining diet + testosterone therapy results in a greater reduction in fat mass (-2.9 kg) and visceral fat, and a reduced loss of lean mass after 1 year.
- Dieting men who receive testosterone therapy display higher physical activity levels than dieting men not receiving testosterone therapy.
- The elevation in testosterone levels by diet alone is not enough to optimize body composition results. Diet alone results in less body fat reduction and more lean mass loss than diet + testosterone therapy.
- Diet + testosterone therapy ameliorates symptoms long-term after a diet. Diet alone does not confer long-term symptomatic improvements.
- Diet + testosterone therapy, but not diet alone, reduces leptin resistance.
Long-Term Testosterone Therapy Improves Cardiometabolic Function and Reduces Risk of Cardiovascular Disease: Real-Life Results
- Published in Testosterone Replacement Therapy
- Written by Monica

Article Tags
Testosterone treatment is NOT associated with risk of adverse cardiovascular events – the RHYME study
- Published in Testosterone Replacement Therapy
- Written by Monica
Article Tags
Testosterone Therapy in Men with Prostate Cancer – Yes or No?
- Published in Testosterone Replacement Therapy
- Written by Monica
Article Tags
How is anabolic steroid use different from testosterone replacement therapy?
- Published in Testosterone Replacement Therapy
- Written by Monica