Is there a protective role of testosterone against high-grade prostate cancer?
Historically, testosterone has almost been a synonym for prostate cancer, and therefore many men have been - and still are - denied testosterone therapy, despite having testosterone deficiency.[1]
A rapidly growing number of studies have challenged the long-standing belief about a putative detrimental association between testosterone and prostate cancer development and/or progression.[2-5] Here I summarize the results of a study published in The Aging Male, which investigated the incidence and severity of prostate cancer in testosterone treated versus non-testosterone treated patients who underwent prostate biopsy.[1]
Key Points
- Testosterone deficient men who receive testosterone therapy have a lower incidence of prostate cancer.
- Testosterone therapy may protect against high-grade prostate cancer.
- Both the development and progression of prostate cancer is lower in men who receive testosterone therapy, compared to untreated men.
What is known
A pervasive concern with testosterone therapy is prostate disease.[1, 6] The fear that higher testosterone level will increase prostate cancer growth originated from a theory of testosterone-dependent prostate cancer growth that was seen in castrated men.[6] This finding is not relevant to testosterone therapy in hypogonadal men; even low testosterone levels that are seen in men with testosterone deficiency are typically above the androgen saturation point (i.e. the level above which further increases in testosterone levels will not affect the prostate because it has already become saturated with androgens).[7]
Contrary to widespread belief, it has been shown that long-term testosterone therapy for up to 17 years does not increase prostate cancer incidence.[8] For more info, see my previous article “Incidence of Prostate Cancer after Testosterone Therapy for up to 17 years”.
When prostate cancer does develop, it is men with low testosterone levels who develop higher grade (more advanced) prostate cancer.[9-13] In fact, data suggest that low testosterone levels, especially low free testosterone, may be a marker for more aggressive prostate cancer.[14-16] More recently, a study showed that low testosterone level is an independent risk factor for high-grade prostate cancer.[17]
The REDUCE trial found no significant association between testosterone levels and prostate cancer diagnosis; among men with the very highest levels of testosterone there was a trend towards a reduced number of prostate cancer diagnoses.[18]
A meta-analysis of 43 studies showed that testosterone therapy for hypogonadism does not increase prostate cancer risk or Gleason grade of cancer detected in testosterone treated vs untreated men.[19] Another meta-analysis of 22 randomized controlled trials concluded that testosterone therapy does not promote prostate cancer development or progression.[20]
What this study adds
In the present study, the incidence and severity of prostate cancer, Gleason scores and tumor staging were assessed in prostate biopsies from hypogonadal men undergoing testosterone therapy, and compared with biopsies from eugonadal men (i.e. men who are not testosterone deficient) and untreated hypogonadal men.[1]
The study was conducted between 2008 and 2013 and included 553 patients. Mean age at biopsy was 61 (range 46–81 years) and PSA 3.7 (range 0.28–7.23 mg/mL). The incidence and severity of prostate cancer was assessed via biopsy in three patient groups presenting at a urology clinic:
(a) 42 hypogonadal men (testosterone level <12.1 ng/dL or <350 ng/dL) receiving testosterone therapy.
(b) 162 untreated hypogonadal men, with a median pretreatment total testosterone level of 7.1 nmol/L or 205 ng/dL (range 3.3 - 11.7 nmol/L or 95 – 337 ng/dL).
(c) 349 eugonadal men.
Biopsies were performed when indicated and following patient consent, according to the European Association of Urology (EAU) guidelines.[21]
As illustrated in figure 1, pathological analysis of prostate biopsies examining the incidence and severity of prostate cancer revealed that:
17% (7 patients) of treated hypogonadal men had a positive biopsy, a Gleason score of ≤6 in 71% and >6 in 29% of men, a predominant score of 3 in all men (100%) and tumor staging of II in 86% men;
52% (84 patients) of untreated hypogonadal men had a positive biopsy, a Gleason score of ≤6 in 41% and >6 in 60% men, a predominant score of 3 (77%) and tumor staging of II (42%) or III (41%);
38% (132 patients) of eugonadal men had a positive biopsy, a Gleason score of ≤6 in 42% and >6 in 58% of men, a predominant score of 3 (83%) and tumor staging of II (45%) or III (48%).
Figure 1: Incidence and severity of prostate cancer in testosterone treated hypogonadal men vs. non-treated hypogonadal men vs. eugonadal men.[1]
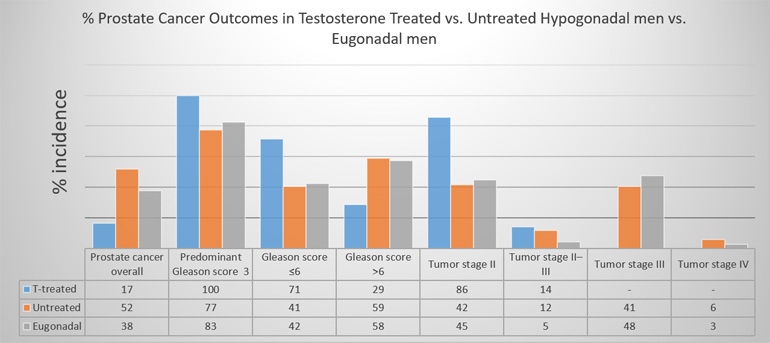
It was concluded that the incidence of prostate cancer was lowest in hypogonadal men receiving testosterone therapy, with significantly lower severity of prostate cancer in terms of staging and grading in the testosterone treated hypogonadal men.[1] These results suggest that testosterone therapy might have a protective effect against high-grade prostate cancer.[1]
Comments
This study shows for the first time that testosterone therapy may protect against both development and progression of prostate cancer in testosterone deficient men.[1] A few days after the publication of this study another study was published, which demonstrated that testosterone therapy for >1 year has been associated with a 56% reduced risk of aggressive prostate cancer (odds ratio = 0.44).[22]
A well-established treatment of prostate cancer is androgen deprivation therapy, which reduces testosterone levels to castrate levels.[23] This has contributed to the belief that since depriving the prostate of testosterone (androgens) reduces growth of prostate cancer, then high levels of testosterone must be bad for the prostate.[6] However, this reasoning is based on “guilt by association” [6] and fails to acknowledge results from more recent studies, which have given rise to the saturation model [7] and the dynamic model.[24]
The dynamic model of the role of testosterone in prostate cancer development postulates that the absolute value of testosterone measured at a single time point is not indicative of prostate cancer risk.[24] Instead, the key factor is the magnitude of the age-related decline in testosterone, from its highest peak in young adulthood to the hypogonadal level where symptoms and signs of testosterone deficiency appear.[24] The risk of prostate cancer increases when testosterone levels fall below a hypogonadal testosterone threshold, which varies between individuals. As testosterone level falls below this threshold, previously healthy prostate cells, now being deprived of testosterone, turn into prostate cancer cells.[24]
The purpose of testosterone treatment is to compensate for the age-related declines in testosterone and to maintain testosterone levels above the threshold, below which the prostate carcinogenesis process is triggered.[24] This explains why the untreated hypogonadal men in the study reported ended up with a higher prostate cancer incidence overall, as well as more aggressive prostate cancer than hypogonadal men who received testosterone therapy.[1] The higher incidence of prostate cancer and aggressiveness in eugonadal men compared to testosterone treated men could have occurred because testosterone treatment in the hypogonadal men achieved higher testosterone levels than those seen in eugonadal men, who despite being classified as eugonadal may have had suboptimal testosterone levels.
The dynamic model of the role of testosterone in prostate cancer development also explains why other testosterone treatment studies found no higher risk of prostate cancer than that seen in the general population.[25-27] Notably, a study published in the Lancet - one of the most prestigious medical journals - showed that the risk of prostate cancer diagnosis was decreased by 40% in men with the longest duration of testosterone treatment (25-51 months). [28] The demonstrated lack of change in prostate histology after testosterone therapy confirms its safety.[27]
While it is well accepted that testosterone therapy is contraindicated in metastatic prostate cancer, the historical fear that testosterone is bad for the prostate has clearly been refuted. As evidenced in this study [1] and explained by the dynamic model of the role of testosterone in prostate cancer development [24], denying or delaying testosterone treatment can actually put men at a significantly increased risk of prostate cancer.
References:
1. Yassin, A., et al., Is there a protective role of testosterone against high-grade prostate cancer? Incidence and severity of prostate cancer in 553 patients who underwent prostate biopsy: a prospective data register. Aging Male, 2017: p. 1-9.
2. Morgentaler, A., Controversies and Advances With Testosterone Therapy: A 40-Year Perspective. Urology, 2016. 89: p. 27-32.
3. Shabsigh, R., et al., Testosterone therapy in hypogonadal men and potential prostate cancer risk: a systematic review. International Journal of Impotence Research, 2009. 21(1): p. 9-23.
4. Boyle, P., et al., Endogenous and exogenous testosterone and the risk of prostate cancer and increased prostate-specific antigen (PSA) level: a meta-analysis. BJU Int, 2016. 118(5): p. 731-741.
5. Debruyne, F.M., et al., Testosterone treatment is not associated with increased risk of prostate cancer or worsening of lower urinary tract symptoms: prostate health outcomes in the Registry of Hypogonadism in Men. BJU Int, 2017. 119(2): p. 216-224.
6. Morgentaler, A., Guilt by association: a historical perspective on Huggins, testosterone therapy, and prostate cancer. J Sex Med, 2008. 5(8): p. 1834-40.
7. Morgentaler, A. and A.M. Traish, Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth. Eur Urol, 2009. 55(2): p. 310-20.
8. Haider, A., et al., Incidence of prostate cancer in hypogonadal men receiving testosterone therapy: observations from 5-year median followup of 3 registries. J Urol, 2015. 193(1): p. 80-6.
9. Cabral, P.H.O., et al., Study of testosterone as a predictor of tumor aggressiveness in patients with prostate cancer. International braz j urol, 2013. 39: p. 173-181.
10. Garcia-Cruz, E., et al., Low testosterone levels are related to poor prognosis factors in men with prostate cancer prior to treatment. BJU Int, 2012. 110(11 Pt B): p. E541-6.
11. Llukani, E., et al., Low levels of serum testosterone in middle-aged men impact pathological features of prostate cancer. Prostate Int, 2017. 5(1): p. 17-23.
12. Pichon, A., et al., Preoperative low serum testosterone is associated with high-grade prostate cancer and an increased Gleason score upgrading. Prostate Cancer Prostatic Dis, 2015. 18(4): p. 382-7.
13. Ferro, M., et al., Low serum total testosterone level as a predictor of upstaging and upgrading in low-risk prostate cancer patients meeting the inclusion criteria for active surveillance. Oncotarget, 2017. 8(11): p. 18424-18434.
14. Hoffman, M.A., W.C. DeWolf, and A. Morgentaler, Is low serum free testosterone a marker for high grade prostate cancer? J Urol, 2000. 163(3): p. 824-7.
15. Salonia, A., et al., Preoperative hypogonadism is not an independent predictor of high-risk disease in patients undergoing radical prostatectomy. Cancer, 2011. 117(17): p. 3953-62.
16. Morgentaler, A., Turning conventional wisdom upside-down: low serum testosterone and high-risk prostate cancer. Cancer, 2011. 117(17): p. 3885-8.
17. Park, J., et al., Low testosterone level is an independent risk factor for high-grade prostate cancer detection at biopsy. BJU Int, 2016. 118(2): p. 230-5.
18. Muller, R.L., et al., Serum testosterone and dihydrotestosterone and prostate cancer risk in the placebo arm of the Reduction by Dutasteride of Prostate Cancer Events trial. Eur Urol, 2012. 62(5): p. 757-64.
19. Shabsigh, R., et al., Testosterone therapy in hypogonadal men and potential prostate cancer risk: a systematic review. Int J Impot Res, 2009. 21(1): p. 9-23.
20. Cui, Y., et al., The effect of testosterone replacement therapy on prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis, 2014. 17(2): p. 132-43.
21. Mottet, N., et al., EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol, 2017. 71(4): p. 618-629.
22. Loeb, S., et al., Testosterone Replacement Therapy and Risk of Favorable and Aggressive Prostate Cancer. Journal of Clinical Oncology, 2017. 0(0): p. JCO.2016.69.5304.
23. Aoun, F., et al., Androgen deprivation therapy in the treatment of locally advanced, nonmetastatic prostate cancer: practical experience and a review of the clinical trial evidence. Ther Adv Urol, 2017. 9(3-4): p. 73-80.
24. Xu, X., et al., Current opinion on the role of testosterone in the development of prostate cancer: a dynamic model. BMC Cancer, 2015. 15: p. 806.
25. Raynaud, J.P., Prostate cancer risk in testosterone-treated men. J Steroid Biochem Mol Biol, 2006. 102(1-5): p. 261-6.
26. Feneley, M.R. and M. Carruthers, Is testosterone treatment good for the prostate? Study of safety during long-term treatment. J Sex Med, 2012. 9(8): p. 2138-49.
27. Efesoy, O., et al., The effect of testosterone treatment on prostate histology and apoptosis in men with late-onset hypogonadism. Aging Male, 2016. 19(2): p. 79-84.
28. Wallis, C.J.D., et al., Survival and cardiovascular events in men treated with testosterone replacement therapy: an intention-to-treat observational cohort study. The Lancet Diabetes & Endocrinology, 2016. May 7.



