Do long-chain omega-3 fatty acids (like those in fish oil) increase prostate cancer risk?
- Published in Diet, Nutrition & Supplements
- Written by Monica

A hotly debated recent study, the SELECT trial, has casted doubt on the well documented health benefits of omega-3 fatty acids. This study found that a higher content of long-chain omega-3 fatty acids (EPA+DPA+DHA) in blood plasma was associated with a greater risk of low-grade (44%) and high-grade (71%) prostate cancers over a 5-year follow-up [1]. Associations were similar for individual long-chain omega-3 fatty acids. Higher linoleic acid (omega-6) was associated with a 25% reduced risk of low-grade and 23% reduced risk of total prostate cancer [1].This has understandably generated confusion among the general public and intense discussions among health professionals and researchers. However, a deeper look at the data and study methodology reveals a different picture...
This has understandably generated confusion among the general public and intense discussions among health professionals and researchers. However, a deeper look at the data and study methodology reveals a different picture...
The Androgen Study Group - Cutting Through Misleading Headlines and Exposing the Truth about Testosterone Therapy and Health
- Published in Testosterone Replacement Therapy
- Written by Monica

Article Tags
Niacin - vitamin B3 - elevates HDL levels (the "good" cholesterol) more than popular medications
- Published in Diet, Nutrition & Supplements
- Written by Monica
Low HDL-C levels are an independent risk factor for development of coronary heart disease (CHD).[1] At all levels of total cholesterol, HDL-C shows a strong inverse association with incidence of CHD. Every 1 mg/dl increase in HDL is associated with a 2-3% decrease cardiovascular risk.[1]
Among men and women aged 49-82 years, who were free of CHD at baseline, after a follow up of 12 yr, the participants with high HDL-C levels (over 60 mg/dL) had half the risk of cardiovascular events compared with participants with low HDL-C levels (below 40 mg/dL).[2] Another large study of 4,500 subjects aged 16-65 years, found after a follow-up of 6 years that individuals with HDL-C levels below <35 mg/dl were at 4 times higher heart disease risk than those with HDL-C levels over 35 mg/dl.[3]
The prevalence of low HDL levels in apparently healthy US adults is 35% in men (defined as below 40 mg/dL or 1.03 mmol/) and 39% of women (below 50 mg/dL or 1.29 mmol/L).[4] Among patients with established cardiovascular disease, 20% to 60% have low HDL levels.[5-7] Furthermore, low HDL levels are part of the criteria for the metabolic syndrome [8] and are highly prevalent among patients with diabetes, affecting more than 50% of men and 66% of women who are diabetic.[9, 10]
Statins are the most commonly used medications for heart disease. However, while statin is the most effective medication to reduce LDL (the "bad" cholesterol) levels, there remains an unacceptably high residual risk in patients who have been on statin treatment. Even after intensive statin treatment that has achieved very low LDL levels, morbidity and mortality rates among statin-treated patients still remain approximately two thirds to three quarters of those found in patients who were getting placebo.[11, 12] This large residual risk clearly indicates that LDL only modestly impacts atherosclerosis at best. Therefore, medical research is investigating HDL elevating treatments with the aim to reduce residual risk, and prevent development of cardiovascular diesase in the first place.
Article Tags
Cheating on a diet - good or bad?
- Published in Diet, Nutrition & Supplements
- Written by Monica

In discussions about dieting, a topic that often comes up is that of "cheating"; is it good or bad to cheat once in a while during a diet?
In order to answer this question appropriately, it is necessary to look at both the quantitative and qualitative aspects of dieting, and the physiological and psychological responses they each elicit...
Dieting - what are we really talking about?
The dictionary definition of "diet" and "dieting" is "to eat and drink sparingly or according to prescribed rules" or "a controlled intake of foods, as for medical reasons or cosmetic weight loss".
However, these definitions do not tell us anything about the two different aspects of dieting; the quantitative and qualitative parts, and their respective consequences. In everyday parlance, dieting usually implies both eating less calories (quantitative aspect) than usual, and eating "specific" foods (qualitative aspect).
Nevertheless, when considering the consequences of "cheating" and trying to answer the question whether it is a good or bad practice, it is important to distinguish these aspects of dieting. Let's take a quick look at each:
Article Tags
Watch Your Waist - it may shorten your life!
- Published in Waist - Abdominal Obesity
- Written by Monica

Your waistline not only makes or breaks your esthetic appearance; if you belly gets too large, it may greatly jeopardize your health and even longevity.
Waist circumference strongly correlates with abdominal obesity and is the most commonly used measure of body fat distribution.[1, 2] Many studies have found enlarged waist circumferences to be associated with all-cause mortality, in most cases independently of general obesity.[3-11]
Abdominal obesity (aka visceral obesity) appears to be more strongly associated with multiple chronic diseases than is gluteo-femoral obesity (fat deposition around the butt and thighs).[1] Increased waist circumference confers a health risk even in normal weight people.[12]
A notable large study investigated the association of waist circumference with mortality using intuitive 2 in (5 cm) increments for men and women, and also evaluated risk within narrow categories of body fatness (BMI). In addition, the study estimated years of life lost due to a large waist circumference.[13]
Article Tags
Multiple Hormonal Deficiencies in Anabolic Hormones in Frail Older Women
- Published in Hormones & Health
- Written by Monica

Reduced levels of anabolic hormones can contribute to aging and frailty. Most studies that have investigated this focused on the relationship between individual hormones and specific age-associated diseases. An interesting study in older women aged 70-79 years sought to examine the associations of individual anabolic hormonal deficiencies of free testosterone, IGF-1 and DHEA, and to assess their combined effects as well.[1]
Article Tags
Relationship between Low Levels of Anabolic Hormones and Mortality in Older Men
- Published in Hormones & Health
- Written by Monica

The anabolic hormones testosterone, IGF-1 and DHEA (a pre-hormone) are receiving more and more attention by health professionals because the anabolic-catabolic imbalance that favors catabolism is a key factor in accelerated physical deterioration aging.[1, 2] Anabolic impairment can speed up the age-related decline in muscle mass and physical performance, increase in fat mass, development of insulin resistance, cardiovascular risk factors, metabolic syndrome and diabetes, conditions that in turn affect mortality.[3-18]
Interestingly, low levels of multiple anabolic hormones, rather than a single one, has a stronger association with age related muscle loss and the frailty syndrome. [19, 20] In men with chronic heart failure, deficiency of more than one anabolic hormone identifies patients with higher mortality rates.[21]
An interesting study sought to investigate the relationship between parallel deficiency of several anabolic hormones and mortality in a general population of older men, regardless of coexisting disease:[22]
Article Tags
Combined Testosterone and GH therapy for best results on body composition and safety profiles
- Published in Testosterone + GH combined
- Written by Monica

Many studies have highlighted the importance of investigating all major hormones, and correcting deficiencies and imbalances if present.[1-8] Given the known mechanisms of testosterone and GH/IGF-1 in building muscle (and possibly also DHEA in elderly) it is reasonable that age-related low levels of anabolic hormones contribute over time to sarcopenia and frailty.[1, 2, 4, 7, 9, 10]
Thus, multiple small effects in aggregate can lead to adverse loss of muscle and disability. In this scenario, if replacement was to occur, it would require lower doses of multiple anabolic hormones. An added benefit to this approach would be fewer side effects from the use of lower hormone doses [11]. In addition, multiple anabolic hormone replacement might also have beneficial additive or even synergistic effects.[11-13]
A notable study investigated whether supplementation with testosterone and GH together, in physiological doses, results in greater improvements in body composition and muscle performance in older men, compared to testosterone supplementation alone...
Article Tags
DHEA supplementation in older adults helps reverse arterial aging

When it comes to health promotion and longevity, DHEA is a supplement which deserves more attention than it has been getting.
DHEA levels (the main circulating form of DHEA in the bloodstream is DHEAS) decrease approximately 80% between ages 25 and 75 year.[1, 2]This large decline in DHEA has led to interest in the possibility that aging related DHEA deficiency may play a role in the deterioration in physiological and metabolic functions with aging, and in the development of chronic diseases.
In support of this, it has been reported that DHEA level is negatively correlated with mortality and risk of developing cardiovascular disease (CVD) (i.e. lower DHEA(S) levels are associated with higher mortality and CVD risk).[3-5]More recently it has been found that a steep decline or extreme variability over time in DHEA(S) levels is associated with higher mortality, more so than baseline DHEA(S) levels.[6]
Aging not only reduces DHEA(S) levels, but also results in an increase in arterial stiffness [7, 8], which is an independent predictor of cardiovascular disease (CVD) risk and mortality.[9-11]
It has been reported that DHEA levels are inversely associated with arterial stiffness (i.e. lower DHEA levels are associated with increased arterial stiffness. [7, 12, 13] Therefore, it is possible that DHEA replacement in older adults could reduce arterial stiffness, and thereby contribute to reduction in CVD and mortality...
Article Tags
DHEA - does it have any beneficial effects beyond testosterone and estrogen action?
DHEA (dehydroepiandrosterone) is most known for being a pro-hormone which in the body gets converted to testosterone and estrogen. It is a long held view that DHEA exerts all its effects via conversion to testosterone and estrogen. However, recent studies show that DHEA also has several health promoting non-hormonal actions...
DHEA 101
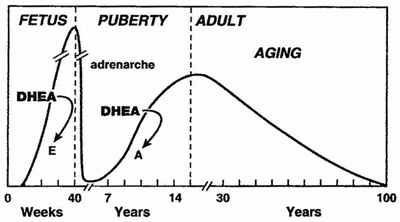
DHEA is produced mainly by the adrenal cortex, and is rapidly sulfated by sulfotransferases into DHEA-S. DHEA and its sulfated form DHEA-S is the most abundant steroid (pro)hormone circulating in the blood stream.[1] The sulfated from of DHEA has a longer half-life in the blood and its levels remain stable throughout the day, are not altered significantly by the menstrual cycle. When getting a blood test for DHEA, the fraction that is routinely measured is therefore DHEA-S. In response to metabolic demand, DHEA-S is rapidly converted back to DHEA (e.g. is hydrolyzed to DHEA by sulfatases).
DHEA levels decrease approximately 80% between ages 25 and 75 year.[2, 3] This large decline in DHEA spurred research interest in the possibility that aging related DHEA deficiency may play a role in the deterioration of physiological and metabolic functions with aging, and in the development of chronic diseases.



