Video Summary: Testosterone Deficiency and Treatment - International Expert Consensus Resolutions
- Published in Testosterone Replacement Therapy

In a previous article "Testosterone Deficiency and Treatment - the FACTS" I presented the conclusions from an International Expert Consensus Conference on Testosterone Deficiency and Its Treatment.[1]
Here I summarize the key points, and link to a video summary by Dr. Abraham Morgentaler, an internationally renowned testosterone scientist and clinician.
Testosterone Deficiency and Treatment - the FACTS
- Published in Testosterone Replacement Therapy
Testosterone deficiency and treatment is a very misunderstood and controversial topic among scientists, regulatory agencies (such as the FDA and EMA) and doctors, as well as the popular media.
On October 1, 2015, an international expert consensus conference about testosterone deficiency and its treatment was held in Prague, sponsored by King’s College London and the International Society for the Study of the Aging Male (ISSAM). The impetus for this meeting was to address the widespread misinformation and confusion about testosterone deficiency and testosterone therapy.[1]
The ultimate goal of this consensus conference was to document what is true or untrue about testosterone deficiency and testosterone therapy, to the best degree possible based on existing scientific and clinical evidence.
There were 18 experts from 11 countries on 4 continents. Specialties included urology, endocrinology, internal medicine, diabetology, and basic science research. Experts were invited on the basis of extensive clinical experience with testosterone deficiency and its treatment and/or research experience.
The final consensus on several key issues related to testosterone therapy was published in the form of 9 resolutions (i.e. firm decisions), coupled with expert comments.[2] These are summarized in table 1.
Real-life experience of continuous long-term testosterone therapy on anthropometric, endocrine and metabolic parameters for up to 10 years
- Published in Testosterone Replacement Therapy
While it is well documented that testosterone levels decline in aging men, recent studies show that in some cases obesity and impaired general health can be more influential causes of testosterone deficiency than chronological age and aging per se.[1, 2]
Here I present real-life results from a registry study which investigated the effects of continuous long-term testosterone therapy for up to 10 years on anthropometric (body measurements), endocrine and metabolic parameters in obese hypogonadal men.[3]
Survival and cardiovascular events in men on testosterone treatment
- Published in Testosterone Replacement Therapy

On the surface, testosterone therapy is a controversial treatment because previous studies investigating the effects of testosterone therapy have been conflicting, with some studies showing supposed harm and others showing significant benefit.
Here I summarize the results of a new study published in The Lancet Diabetes & Endocrinology on May 7 2016, which addressed some shortcomings in previous studies by analyzing effects based on duration of testosterone treatment.[1]
Everything We Learned About TESTOSTERONE Is WRONG - video presentation by Dr. Morgentaler
- Published in Testosterone Replacement Therapy
Historically testosterone therapy was only indicated in men with pituitary tumors and testicular dysfunction. Dr. Morgentaler pioneered the field when he started to treat men – who did not have any underlying pituitary tumors and testicular dysfunction - with Low-T with testosterone therapy. His patients reported improved erections, libido, orgasm, as well as increased energy, mood, cognition and wellbeing.
This use of testosterone therapy in otherwise healthy men defied standard medical practice in the 1990s...
Testosterone levels, testosterone therapy and all-cause mortality in men with type 2 diabetes - impact of PDE5 inhibitors and statins
- Published in Testosterone Replacement Therapy

The prevalence of testosterone deficiency is higher in men with type 2 diabetes than among non-diabetic men [1-6], and testosterone deficiency is associated with increased mortality.[7, 8]
Type 2 diabetic men often have dyslipidemia [9] and erectile dysfunction [10, 11], and hence statins and phosphodiesterase 5 inhibitors (PDE5I) are widely used in these men.
Here I summarize the results of a study published in International Journal of Clinical Practice, which investigated the impact of testosterone levels and testosterone therapy on mortality, and assessed if this was affected by concomitant statin and PDE5I use.[12]
Effects of Testosterone Treatment in Older Men
- Published in Testosterone Replacement Therapy

The so called double-blind randomized controlled trial (RCT) is accepted by medicine as the gold standard objective scientific methodology, and provides the highest strength of evidence for the effectiveness of a treatment.[1-4]
An accumulating body of evidence shows that treating hypogonadal men with testosterone therapy provides a number of wide-ranging benefits beyond mere relief of symptoms, including improvements in muscle mass, insulin sensitivity, fat mass (both total body fat and visceral fat), endothelial function, blood pressure, lipid profile and bone mineral density.[5, 6]
Recent clinical practice guidelines state that testosterone therapy is safe if treatment and monitoring are appropriately executed [7-9], and the totality of available evidence to date does not support alleged concerns regarding risk of cardiovascular disease [10] and prostate cancer.[11] Despite this, opponents state that the clinical benefits and potential long-term risks of testosterone therapy have not been adequately assessed in large RCTs, and that therefore a general policy of testosterone replacement in all older men with age-related decline in testosterone levels is not justified.[12]
To address the lack of large RCTs on testosterone therapy, the US National Institute of Health has funded The Testosterone Trials, which is a coordinated set of 7 large double-blind RCTs. Here I report the first results from The Testosterone Trials, which were released February 18, 2016.[13]
Effects of long-term testosterone treatment on weight loss and waist size in obese men - is TRT the next obesity treatment?
- Published in Testosterone Replacement Therapy

Testosterone, historically believed to be important only for male reproduction and sexuality, has over the past decades transformed from niche hormone to multi-system player.[1] A rapidly accumulating body of research is showing that testosterone is an important metabolic hormone with marked effects on energy metabolism and body composition.[2]
In USA, 36% of the adult population are obese (BMI >30), (affecting a similar proportion of men and women) [3], and obesity prevalence is escalating worldwide. According to the McKinsey Global Institute (MGI) report “Overcoming obesity: An initial economic analysis”, obesity is “one of the top three preventable social burdens (along with smoking and violence/war/terrorism) generated by human beings” imposing an estimated annual global direct economic burden amounting to 2 trillion USD.[4]
Obesity treatments with comprehensive lifestyle modification and/or drugs are notorious for their poor long-term efficacy and inability to achieve long-term weight loss maintenance.[5-9] Even with continued lifestyle treatment, significant weight regain occurs.[7, 9, 10] And obesity drugs have side effects which limit their long-term and widespread use. [11, 12] Therefore, new interventions are urgently needed to combat this alarming preventable threat to society.
Here I summarize a recent study that investigated the effects of long-term testosterone treatment – up to 8 years - on weight loss and waist size in 411 testosterone deficient men with obesity classes I-III.[13]
Critical Update of the 2010 Endocrine Society Clinical Practice Guidelines for Hypogonadism
- Published in Testosterone Replacement Therapy

In 2010, the Endocrine Society published a Clinical Practice Guideline “Testosterone Therapy in Adult Men With Androgen Deficiency Syndromes”, which addressed important issues regarding the diagnosis and treatment of male hypogonadism.[1]
Since publication of this Guideline, several high-quality trials have been conducted, warranting an update of the 2010 recommendations in several areas, especially that of testosterone therapy in men with the metabolic syndrome, type 2 diabetes, sexual dysfunction, and frailty.
In addition, many of the previously stated contraindications to testosterone therapy – including severe lower urinary tract symptoms (LUTS) and untreated obstructive sleep apnea (OSA) - have been reexamined in recent trials.
Here I summarize the results of a recent systematic analysis of the latest high-quality studies, which call for some important updates of the 2010 Endocrine Society Clinical Practice Guidelines for Male Hypogonadism.[2]
Effects of Testosterone Therapy for 3 Years on Subclinical Atherosclerosis Progression in Older Men
- Published in Testosterone Replacement Therapy
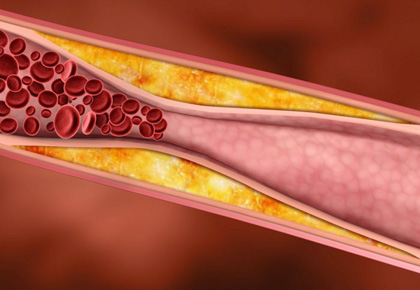
Clinical practice guidelines rely heavily on results from randomized controlled trials (RCTs), which is the gold standard for medical research. RCTs produce evidence considered to be of the highest quality. Because RCTs are resource intensive and costly, they are typically of relatively short duration, commonly lasting for around one year.
Currently there are only a few placebo-controlled RCTs investigating the effects of testosterone therapy for a duration of 3 years [1-4], and medical societies have long been urging for more long-term trials evaluating the safety and efficacy of testosterone therapy.[5-7]
On August 11th 2015 a notable 3-year long RCT was published in JAMA (Journal of the American Medical Association), which attracted a lot of attention.[8] While interpreted by many as showing that testosterone therapy does not confer any benefits on atherosclerosis, sexual function and quality of life, a closer look at the data actually shows two important positive results…



