New Approach to Treat PD with Regenerative Medicine
Investigation on finding alternative solutions to present treatments for patients has led to regenerative medicine. This type of medicine includes use of a different approach to treat orthopedic injuries, pain management, and certain disorders utilizing platelet rich plasma, adipose, bone marrow, and umbilical cords 1. Research in recent years has discovered significant advancements in the methods to harvest human mesenchymal stem cells (MSCs) for its potential treatment to fibrosis. Stem cells are unspecialized entities that are capable of transforming into different types of cells, such as muscle, brain, skin, or red blood cells and may help mitigate excessive scar tissue in a much less invasive method. As new tests are conducted in different fields of medicine, use of MSCs have become more and more prevalent in fighting disease including Peyronie’s disease due to their unique ability to be specifically induced.
Mesenchymal Stem Cells (MSC)
Similar to other fibrotic diseases, the cause of Peyronie’s disease (PD) is still unclear. This disease is defined by fibrous plaque that accumulates on the soft tissue of the male sexual organ; this causes the organ to bend significantly as well as cause erectile dysfunction, followed by pain and difficulty in sexual performance. Even with the current wide array of medications, procedures, natural remedies, and alternative options available, finding effective treatment of Peyronie’s disease remains a challenge to this day.
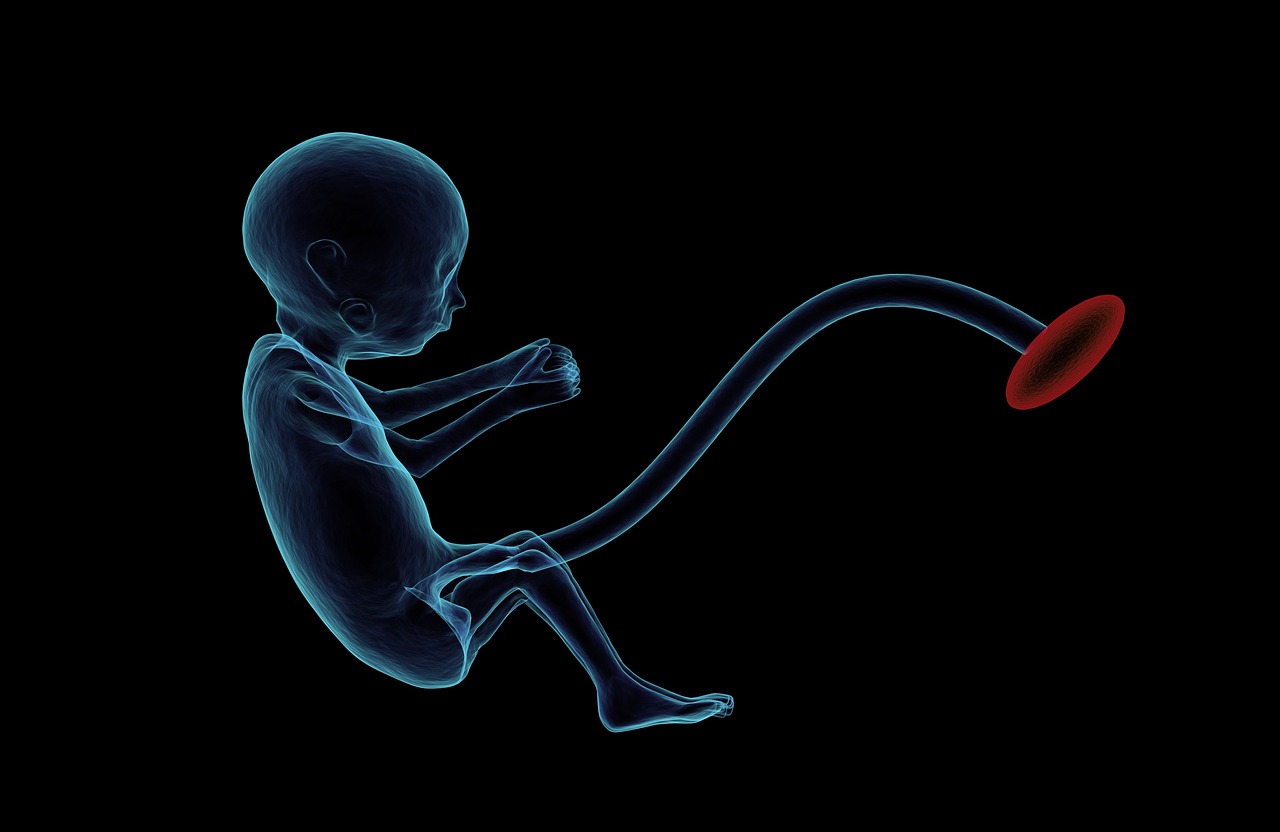
Umbilical Cord Matrix (UCM) - A Potential Plentiful Source of MSC
The human umbilical cord matrix (UCM) appears to be a potential source of MSC due to its non-controversial nature1. Compared to embryonic stem cells, UCM is considered an incontestable source of primitive stem cells and unlike bone marrow stem cells, UCM offers a painless collection procedure and shorter timespan for self-repair; this is ideal for treating a sensitive area such as the male sexual organ for PD. UCM demonstrates the ability to differentiate into three separate germ layers to stimulate tissue restoration, and regulates immune system responses and anticancer properties.
Wharton’s Jelly
Stem cells can be obtained from the Wharton’s jelly, cord lining, and perivascular region from of the umbilical cord which grows to approximately 50 centimeters in length. As the embryo forms, primitive cells travel between the area of the umbilical cord formation and the embryo. Some of these cells dwell in the matrix during UC development and even remain after giving birth. Research suggests Wharton’s jelly as the leading source of primitive allogeneic MSCs that are able to be obtained from the umbilical cord immediately after the egg has been fertilized 2. There are two types of methods for isolating Wharton’s jelly: the explant approach and the enzymatic digestion approach. The explant approach involves removing the umbilical cord vessels and manually cutting the Wharton’s jelly into 1-2mm3 particles 3. The particles are left undisturbed for a period of a week to enable the stem cells to emerge. However, the particles often float in the medium using this method which fails to provide a consistent number of mesenchymal stem cells 3. The enzymatic digestion approach utilizes the digestive enzymes which provides consistent homogenous cell populations to obtain an abundant number of stem cells than the explant approach 3. Most studies currently use stem cells isolated from Wharton’s Jelly and the results have indicated these cells from Wharton’s jelly may be able to serve many future therapeutic research and clinical application roles.

Predictive Anti-Aging MSC Study and Peyronie’s Disease
Tissue regeneration and maintenance is dependent on stem cells, including MSC. However, recent evidence has shown MSC properties will decline with age considering their use in research for regenerative therapy. After extensive research on the biology of aging and stem cells, aging has been shown to progressively decline in stem cell functionality, offering less effective tissue for regeneration and repair which is a profound fact in our regenerative capacity4. Unfortunately, contemporary data collected of PD suggests the disease commonly occurs in older men between ages 50-55 which may offer less effective results using MSC injections. It is important to understand the significant implications of age-related stem cell dysfunction for regenerative medicine to help manage PD as research continues.
Studies using Stem Cells to Treat Peyronie’s Disease
Studies have been performed on rats to determine the effects of stem cell treatment in Peyronie’s disease. Adipose tissue-derived stem cells were injected into the rat models with PD and the results significantly improved the symptoms of erectile dysfunction 5. Another study conducted at a private clinic between 2013 - 2015 involved human participants with PD ages 18 and older with the exclusion of certain conditions 6. Stem cells were injected into the shaft of affected patients’ sexual organ using a needle to straighten the organ and improve the connective tissue’s elasticity 6. The study only included 5 patients but the effects were statistically significant and promising. The penile curvature dramatically improved at the 6-week, 3-month, and 6-month check ups after injection 6. Because the sample was small, the findings in the study needed to be replicated with a larger sample size. However, this was the first feasible study on the use of stem cells to manage PD in humans and shows major hope for further studies in the future to confirm its efficacy.
Although Peyronie’s disease still remains a challenge and has been a physically and psychologically devastating issue for approximately 9% of men that often worsens over time, regenerative medicine using stem cell research as an alternative treatment for fibrosis and other diseases may have a breakthrough in medicine in the near future. Stem cells may be highly effective in inflammatory scarring conditions such as PD. UCM-MSC through Wharton’s jelly may be the perfect candidate to stimulate tissue restoration and regeneration, offering a much less invasive non-surgical option while providing quicker recovery for patients 1. Another alternative type of non-surgical therapy that may help improve erectile dysfunction and PD is GAINSWave Therapy using low-intensity extracorporeal shockwaves. This shockwave therapy has actually been around for almost two decades but fairly new to the US and Canada market. Benefits using GAINSWaveTM include improved blood flow, erection quality, and sexual performance. As further research is done to understand the cause of PD and other fibrotic diseases along with abilities and limitations exploring non-surgical alternative solutions such as stem cell and shockwave therapy, this may help provide many other biotechnological benefits in the future.
For more information, be sure to check out our Ageless Forever news blog for other health-related articles posted weekly!
References:
1. Predictive Biotech. (2017) [Brochure] Recover. Rebuild. Renew. N.P.: n.p.
2. Zeddou M., Briquet A., Relic B., Josse C., Malaise M., Gothot A., Lechanteur C. and Beguin Y.. The umbilical cord matrix is a better source of mesenchymal stem cells (MSC) than the umbilical cord Blood, 2010. P. 693
2. C. Thomas Vangsness Jr., M.D., Hal Sternberg, M.D., and Liam Harris, B.S. Umbilical Cord Tissue Offers the Greatest Number of Harvestable Mesenchymal Stem Cells for Research and Clinical Application: A Literature Review of Different Harvest Sites, 2015. P. 1836
3. Hassan G., Kasem I., Soukkarieh C., and Aljamali M. (2017, November 10) Simple Method to Isolate and Expand Human Umbilical Cord Derived Mesenchymal Stem Cells: Using Explant Method and Umbilical Cord Blood Serum. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5741200/
4. Bellantuono I. Aging of marrow stromal (skeletal) stem cells and their contribution to age-related bone loss. Biochim Biophys Acta, 2009. 1792: p. 364-370.
5. Castiglione F., Hedlund P., Van der Aa F., et al. Intratunical injection of human adipose tissue-derived stem cells prevents fibrosis and is associated with improved erectile function in a rat model of Peyronie’s disease. Eur Urol. 2013; 63(3): 551-560.
6. Levy J., OMS III, MS; Marchand M, PA-C; Iorio L., OMS I; Zribi G; Zahalsky M. (2017, October). Effects of Stem Cell Treatment in Human Patients With Peyronie Disease. Retrieved from http://jaoa.org/article.aspx?articleid=2445317
